Blog post -
Stopping Sepsis in its Tracks
Sepsis is a more common reason for hospital admission than heart attack - and has a higher mortality.
The most common causes of severe sepsis are pneumonia, bowel perforation, urinary infection, and severe skin infections. The most common signs of sepsis are a high fever, violent shivering, fainting, cold and pale hands, rapid breathing, confusion or delirium.
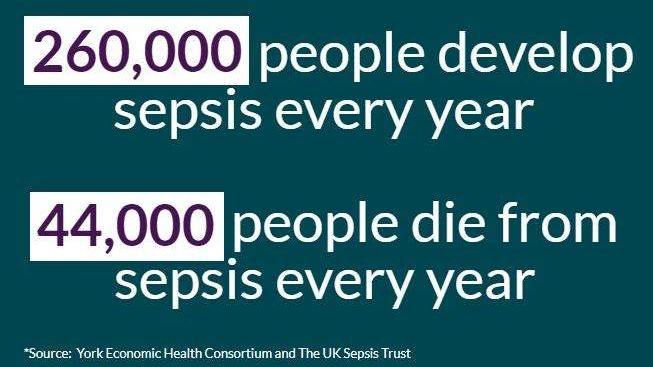
Sepsis is one of our biggest killers. The UK Sepsis Trust states that sepsis claims 44,000 lives every year in the UK and costs the NHS £2.5 billion a year. In comparison, breast cancer claims less than 8,000 lives a year.

The world must face the fact that despite the advances of modern medicine, the fight against infectious diseases and sepsis is far from won. Despite the shocking statistics highlighted above, the public is largely ignorant of the fact that sepsis – also called septicaemia or “blood poisoning” – can be triggered by almost any infectious disease and is responsible for almost 8 million annual deaths worldwide. The annual increase of sepsis cases in industrial nations by 7 – 8% over the last decade has gone largely unnoticed and unremarked.
We need to reduce the catastrophic deaths, life-altering consequences, and high costs of sepsis, but this can only be done by acting quickly to diagnose and treat it in the early stages when symptoms first arise.
Campaigners want to reduce sepsis cases by 20 per cent by 2020 and make the word sepsis a ‘household name’, but in order for us all to achieve this, more has to be done.

Existing research clearly highlights early detection of patient deterioration is vital to improving patient safety and avoiding preventable deaths.
One solution to this is remote monitoring systems that use wireless, sensing and information technologies to continuously collect and analyse patient data, especially from those patients deemed clinically to be most at risk of contracting sepsis. Research shows that subtle variations in the patterns of a patient’s vital signs such as heart rate, respiration rate and temperature indicate the early onset of sepsis and other inflammatory conditions.
‘The Isansys Patient Gateway uses vital sign data, early warning scores and data analytics to flag up any changes in a patient’s condition and detect the early onset of sepsis fast.’


These remote monitoring systems show particular promise in addressing issues related to in-hospital patient safety, as well meeting the needs of patients and providers who wish to extend higher acuity care out of the hospital into the home.
Predictive analytics based on the continuous data and changes in the vital sign patters can help meet the challenge of simple, non-specific screening and early warning indicators. The use of smart, sophisticated algorithms is encouraged to support clinical teams in rapid identification and early intervention.
Isansys Lifecare Ltd, based in Oxfordshire, won a £1 million SBRI Healthcare development contract to develop its Patient Status Engine (PSE), a new class IIa, CE-marked patient monitoring platform which collects and analyses patients’ vital signs and will alert doctors and nurses if a person’s health is deteriorating.
The PSE uses wireless body-worn sensors, including the Isansys Lifetouch, the Isansys Lifetemp and third-party devices to collect patient data. It collects heart rate, respiration, heart rate variability, temperature, oxygen saturation and blood pressure continuously and wirelessly. The platform then uses the vital sign data, early warning scores and data analytics to flag up any changes in a patient’s condition and alert clinicians to what could be the early onset of sepsis fast.
Research shows subtle changes in a patient’s health status is often linked with a sepsis diagnosis including fast breathing, increased heartbeat, change in heart beat pattern and a high or low temperature. Due to the integrated nature of the PSE, these parameters are monitored continuously by the platform. If any one of the parameters register an abnormal level a patient is deemed at risk of developing sepsis. The clinician is then alerted to a change in the patient’s condition and they can react much more quickly than they would be able to otherwise.
Isansys is currently working with the Queen Elizabeth Hospital, Birmingham, where it is working with the clinical team to use data from the PSE to develop an early warning score for patients who have undergone chemotherapy and are at high risk of neutropenic sepsis.
Isansys is working with the Queen Elizabeth Hospital, Birmingham, on the early detection of sepsis

This work is an unprecedented opportunity for Isansys to show the ability of the PSE platform to capture and analyse data from multiple patients in multiple remote locations. The team at Isansys believe this to be the first time that such high resolution patient data will be captured from such high risk, potentially acute, patients in the community.
Results from the project at the Queen Elizabeth Hospital, Birmingham are due to be reported soon but there are already indications of:
Earlier, lower cost and less traumatic interventions
Halting the progression of sepsis in its early stages, potentially allowing more patients to be successfully treated for neutropenic sepsis without requiring admission to the hospital
Presentation of early warning to the patient and (remotely) to the care team
Reducing hospital stay for those who are admitted and significantly improving outcomes
Early detection of patient deterioration is vital to improving patient safety and avoiding preventable deaths. Failure to rapidly diagnose and treat severe sepsis can have tragic consequences.