Blog post -
Sepsis can be detected and treated early with new wireless patient monitoring technology
Sepsis patients can be diagnosed and treated earlier with the help of new technology available for patients in any healthcare setting including hospitals, care homes, and even patient’s own homes.
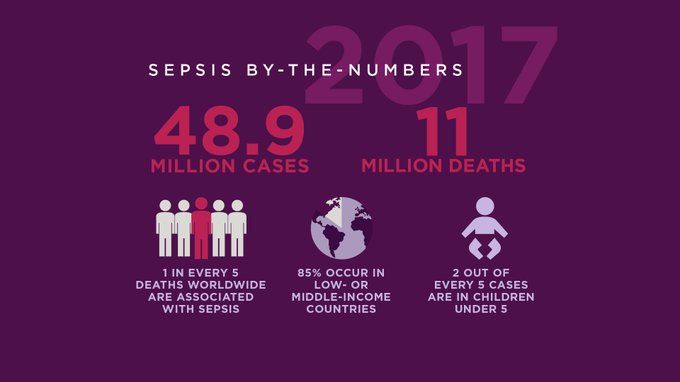
Researchers writing in the Lancet medical journal have found that one in five deaths around the world is caused by sepsis, also known as septicaemia or blood poisoning.The report estimates 11 million people a year are dying from sepsis - more than are killed by cancer.
Deaths from sepsis around the world are twice as high as previously thought, with babies and small children in poorer countries at greatest risk, a major study has revealed.
The researchers at the University of Washington said the "alarming" figures were double previous estimates and that most cases were in poor and middle-income countries, but even wealthier nations are having to deal with sepsis.
In the report it states that reducing the number of infections can reduce the number of cases of sepsis. For many countries, this means good sanitation, clean water and access to vaccines.
The other challenge is to get better at identifying patients with sepsis in order to treat them before it is too late. Early treatment with antibiotics or anti-virals to clear an infection can make a massive difference.
Mohsen Naghavi, Professor of Health Metrics Sciences at the Institute for Health Metrics and Evaluation (IHME) at the University of Washington, said: "We are alarmed to find sepsis deaths are much higher than previously estimated, especially as the condition is both preventable and treatable. We need renewed focus on sepsis prevention among newborns and on tackling antimicrobial resistance, an important driver of the condition."
One solution to this is to use improved patient monitoring systems that use wireless, sensing and information technologies to continuously collect and analyse patient data, especially from those patients deemed clinically to be most at risk of contracting sepsis. Research shows that subtle variations in the patterns of a patient’s vital signs such as heart rate, respiration rate and temperature indicate the early onset of sepsis and other inflammatory conditions.
The Patient Status Engine (PSE), a wireless monitoring system designed and developed by Isansys Lifecare in Oxfordshire, UK, uses body-worn sensors to collect vital signs automatically, continuously and in real-time. The platform then uses this data to flag up any changes in a patient’s condition and alerts clinicians to what could be the early onsets of sepsis faster than they would have otherwise been able to detect it. The PSE addresses issues related to in-hospital patient safety, as well as meeting the needs of patients and providers who wish to extend higher acuity care out of the hospital into the home.
Keith Errey, CEO of Isansys, said: “Being able to identify patients at the highest risk of deterioration is key for us and the clinicians we are working with. The PSE provides earlier indications of patient deterioration than can’t be achieved with manual monitoring alone. This is invaluable in the global fight against sepsis.
“Not only does the PSE provide early warning scores and alerts when a patient’s vital signs significantly change but it also allows the real-time remote monitoring of patients’ responses to treatment. This enables timely interventions which enhance the care and safety of patients in any location.”
Isansys is currently working with the Northwell Health Group in New York. Physicians at the Cohen Children’s Medical Center have carried out a major study using the PSE to monitor mothers during labor to investigate whether maternal fever is a predictor of early onset neonatal sepsis.
Using the PSE, doctors at the US hospital have discovered that continuous measurement of maternal temperature during labor may be a better indicator of high-risk infection in newborn babies compared to standard obstetrical practice of measuring oral temperature. They also discovered that continuous measurement of temperature during labor can detect times when significant fevers are missed by manual oral measurements.
Further work by the Northwell team includes a full analysis of the other continuous vital signs collected during the study such as heart rate, respiration rate, and heart rate variability, and the use of the PSE to monitor neonates.